What? You don't have Idraparinux?
 What kinds of medications are available at an African mission hospital, and from whom do you procure them? These are questions that we get asked a lot. Here are two lists. Five things we have, and five things we don't! Most of our medications are imported from Europe and Asia. A few are made locally in Ethiopia. One thing we can't use is expired meds - it's prohibited by law - so even though we'd like to take these off your hands, please don't send them to us!
What kinds of medications are available at an African mission hospital, and from whom do you procure them? These are questions that we get asked a lot. Here are two lists. Five things we have, and five things we don't! Most of our medications are imported from Europe and Asia. A few are made locally in Ethiopia. One thing we can't use is expired meds - it's prohibited by law - so even though we'd like to take these off your hands, please don't send them to us!
Five medications we have:
- Most antibiotics! We have penicillins, 3rd generation cephalosporins, macrolides, aminoglycosides, fluoroquinolones. We even have vancomycin most of the time.
- Pain meds: For mild pain, we carry ibuprofen and tylenol. We also have stronger IV pain meds for our surgical patients, and fractures.
- Blood pressure and diabetes medications. We have oral calcium channel blockers, ACE inhibitors, diuretics, and some beta-blockers. We use metformin and glibencamide for diabetes control, and we also have insulin.
- Albuterol multi-dose inhalers. These are key for our chronic asthma patients, and COPD patients. We don't have nebulized albuterol (which we'd like to have), but we can substitute these MDIs, and they work quite well.
- GI problems? We've got proton pump inhibitors (Prilosec for example), and we even have Zofran for nausea and vomiting.
Five medications we don't have. We are hoping that in time, our access to some of these meds will improve:
- Fancy antibiotics. Anti-pseudomonal penicillins like Timentin and Zosyn. These are great for severe infections. Also, we still lack a good IV first generation cephalosporin.
- Artesunate. This is the WHO-recommended standard for IV treatment of severe malaria. It is difficult to find however, and we rarely have it. Instead, we use Quinine which is an acceptable but less desirable medication.
- Newer blood pressure and heart failure medications like Carvedilol. Also, newer diabetes meds like long-acting insulins.
- Low-molecular weight heparin. Ever heard of Lovenox? It makes treating deep venous thrombosis and pulmonary embolism so much easier. But alas, it is rarely available on the African market.
- IV calcium and sodium bicarbonate - rarely we will have these. It does create problems managing a hyperkalemic patient or profoundly hypocalcemic patient. We have other therapies that we can use though.
Others you are wondering about? Ask in the comments and we'll respond!
Welcome Home!


There's no place like home! And now, after many years of prayer and preparation, the new Soddo PAACS apartment building is complete, and our residents have moved in to their new homes.
The finished building has 7 apartments (1 three-bedroom, 3 two-bedrooms and 3 one-bedroom apartments). These new apartments will allow the surgical residents to have a reliable source of power and water. And, since they are on the hospital's campus, it will significantly improve their home security, including that of their families. From an educational standpoint, this will also allow us to improve the residents' experience with night call. This will allow senior residents to take back-up call in the night and gain experience in teaching junior residents under faculty supervision in the night hours.
We want to extend our deep appreciation to everyone who gave so graciously to make this happen. We have been encouraged by everyone's support and gifts, even in the end as we raised money to furnish each apartment. A big thank you goes to Africa Mission Healthcare Foundation for their donation that funded over a third of the project costs!
The residents are enjoying living in the same building and often eat together, sing praise music together and enjoy holidays together since they are away from their extended families. Dr. Surafel said, "Living on-campus together gives us lots of time for fellowship and we eat many meals together. It is also easier to see patients more quickly."

playground!

White Coat Ceremony
What is a white coat ceremony, you ask? Well, according to Wikipedia, it is the ritual that marks the transition of a student of medicine from the pre-clinical years to the clinical years. The white coat has been worn for over 100 years by medical professionals, and is clearly associated with the trade. Everyone likes ceremonies, and for doctors, this is an important ritual that bestows the rights as wells as responsibilities on new doctors.
Though typically done with medical students, we have developed our own version of the white coat ceremony for our PAACS residents. Performed as they begin their five year training, we assemble in the chapel here at Soddo Christian Hospital and deliver a charge to the new young surgeons. This past week, we welcomed Dr. Gezahegn and Dr. Ebeneezer into the ninth class of surgical residents here. Here is how it happened:


The time was opened with a song and prayer led by Pastor Daniel, SCH’s head chaplain. Then Dr. Gray read John 13 reminding all of the servant leadership by Jesus and do likewise. “For I have given you an example – you should do just as I have done for you.” John 13:15. Dr. Mark Karnes shared his prayer for the residents from Colossians chapter 1. He charged them with 3 important things to remember throughout their training. First, God is in control; rest and trust in this. Second, treat all patients with care and compassion as if they were family. Third, know your limits and don’t be afraid to ask for help.
Next, Dr. Seigni Bekele, SCH’s chief resident encouraged the interns with some scripture and words of wisdom. He read from Hebrews 12:1-2, mentioning the men of faith that are listed in the chapter before this. He emphasized that there are many people of faith who pray continually for PAACS and for the residents here. He challenged the interns to remember they are a part of something great and many people have gone before them in sacrifice and prayer to get the program to where it is today. And for that we are thankful and give glory to God. “Keeping our eyes fixed on Jesus, the pioneer and perfecter of our faith.” Hebrews 12:2

Dr. Gray spoke last pointing out that in order to be the greatest we need to be the least. And that the desire in us to be the greatest is not wrong, but it is what we are aiming for that makes the difference. If we stay focused on eternity and we strive to do well for the eternal, then the world may consider us crazy, but we will know we are aiming for something great.
Finally, following Jesus' example from John 13, Dr. Karnes and Dr. Gray washed the feet of Dr. Gezahegn and Dr. Ebenezer. Not something you'd find in most white coat ceremonies, but servant leadership being the focal point of our training, a practice that we feel is essential to this rite of passage. As staff physicians, we want to model servant leadership to even our newest trainees, as we begin to mentor them. A blessing was prayed over them as we concluded the ceremony.

Feeding the Soul
Look at all those onions!
These are three of our committed kitchen workers at SCH. Our hospital is unique in that we provide three meals a day to our patients (at other hospitals, the patients’ families have to bring the food), and this is a critical part of getting them healthy. In addition to providing great food, kitchen staff meet in two Bible St.udy groups weekly. They just completed a study on maturing in Christ. When asked how the study has impacted their lives, here were some of the answers:
“We used to get angry easily in the kitchen. Now we understand that this is wrong.”
“Before, I didn’t want to give to the poor. Now I have compassion. My heart is broken and I try to help them.”
“Now sometimes we will even cook food for the patients’ families too.”
One of the groups collected money for two poor patients in the hospital in order to help them pay for transportation costs home from the hospital. Praise God for how He is using these women, and how He is transforming their hearts!
Another Surgeon For Ethiopia
This is a guest post from Dr. Jon Pollock, originally featured on his personal blog. Dr. Pollock is a staff surgeon at Myungsung Christian Medical Center in Addis Ababa, our sister hospital. Our surgery residents, including Dr. Daniel Gidabo, train at both facilities: here in Soddo and at MCM in Addis. (In fact, Dr. Pollock himself previously served as one of our staff surgeons here!) The following is his account of Dr. Daniel's graduation:

Last Saturday, we celebrated the graduation of the sixth PAACS resident in Ethiopia. Dr. Daniel Gidabo finished his five years of training in general surgery at the end of August. Daniel has taken a position as a surgeon in his hometown, a city of more than 100,000 people that has not had a full time surgeon in a very long time. There Daniel will have the opportunity to treat hundreds and thousands of people who otherwise would have died without surgery. We are very proud of Daniel and his accomplishments. He has a well deserved reputation as a bold and effective evangelist and has led literally hundreds of people to Christ during our time with us.

During my remarks at his graduation ceremony, I spoke to Daniel from Psalm 34, one of my favorite Psalms. It begins with triumphant words of praise.
I will extol the Lord at all times;
His praise will always be on my lips.
My soul will boast in the Lord;
let the afflicted hear and rejoice.
Glorify the Lord with me;
let us exalt his name together.
These words were particularly appropriate for this day. We praise God for what he has done for us. When Daniel started his training five years ago, he had no guarantees that his work would amount to anything. The PAACS program in Ethiopia was not accredited at that time. There was little hope that this little upstart program would ever amount to anything. Fast forward five years and we are accredited by both the Ethiopian Ministry of Education and the Ministry of Health and the College of Surgeons of East, Central and Southern Africa. We have expanded from one hospital to two and have tripled the number of residents in the program. This is only because of what God has done to bless the work he has called us to do. Praise God for what he had done. I sought the Lord, and he answered me;
He delivered me from all my fears.
I assured Daniel that there will be times that he will be afraid. Fear is an integral part of being a surgeon, particularly in the first year starting out on your own in practice. I urged him to seek after the Lord, and He would deliver him from all his fears. Delivery from fears comes with another promise if we look to him.
Those who look to him are radiant;
their faces are never covered with shame.
I encouraged Daniel to look to Him and be radiant.
This poor man called, and the Lord heard him;
He saved him out of all his troubles.
I reminded Daniel that his hometown has been without a surgeon for years and that people were crying for help.
Taste and see that the Lord is good;
blessed is the man who takes refuge in him.
As PAACS surgeons, this is as essential to our lives as anything we do in the operating room. We have the unbelievable privilege to invite people to “taste and seek” that the Lord is good. I encouraged Daniel to continue to be bold in his witness.
The righteous cry out, and the Lord delivers them;
He delivers them from all their troubles.
The Lord is close to the brokenhearted
and saves those who are crushed in spirit.
Finally, I told Daniel that as surgeons in Ethiopia, if we let ourselves, our hearts will be broken and our spirits crushed. There are so many challenges, so much pain and disease, so much death that if we are not careful, we can become hardened and uncaring. But as painful as it can be, we must allow our hearts to remain soft and able to be broken, because the pain, disease and death that we face everyday, breaks the heart of God.
One in a Million Babies
 One in 729,000. That is the odds of having quadruplets naturally - without the aid of fertility medicines. And for this young Ethiopian lady, it happened 5 days ago. With no prenatal care, and no knowledge of the multiple babies she was carrying, she made the trek from her rural home to the local health center. There she gave birth to four babies, one of whom died soon after birth.
One in 729,000. That is the odds of having quadruplets naturally - without the aid of fertility medicines. And for this young Ethiopian lady, it happened 5 days ago. With no prenatal care, and no knowledge of the multiple babies she was carrying, she made the trek from her rural home to the local health center. There she gave birth to four babies, one of whom died soon after birth.
She was advised to seek further care at a hospital, and found her way to us. The mother herself is being treated with antibiotics for a suspected uterine infection, but she is expected to make a full recovery. The three surviving kids are doing well. Two of them have a mild omphalitis (an infection of the umbilical cord stump) and are being treated with IV antibiotics. They are expected to do well.
The three celebrated the Ethiopian New Year yesterday on their fourth day of life. The new family is the talk of the hospital as we ring in the New Year. A multiple gestation pregnancy is high-risk in any country, but especially here where over 90% of the women have no access to prenatal care. Though we mourn the loss of one of the babies, we praise God for the miracle of a healthy mom and three healthy infants.
A Miracle at Soddo

The parents were shrieking in grief and disbelief as they ran their 14 month old little boy to the ER at Soddo Christian Hospital.
Just minutes earlier they had found him upside down in a bucket. A bucket of mop water. He had wandered out and managed to tip himself into it, and couldn't get out. He literally drowned.
When the parents brought in little Yekebesera, they thought he had been underwater for at least five minutes. In the ER, he was having seizures which were requiring multiple doses of strong medications to stop them. Only minutes later, he began "posturing" - meaning that he was extending his arms and legs in such a way that indicates very severe brain damage.
Our pediatrician admitted him to the ICU, and assisted his breathing with a CPAP machine which we just purchased through generous donors. All of the doctors who cared for him that evening thought this little boy would never make it. But trusting God, and hoping for a miracle, we did everything we were capable of doing.
The next days, Yeke remained seizure-free, and started waking up more. Here's what our pediatrician Dave Ayer said when he walked into the room on hospital day #3:
"When I came in Sunday morning and his dad asked me if he could eat...I thought he was joking. That is, until I looked down and found out this little guy had purposefully ripped off some of his monitoring equipment. He was interacting normally with his parents and requesting something to drink. It nearly brought me to tears--today he came off CPAP and is on minimal oxygen support and eating/drinking like a normal kiddo. My only remaining challenge will be to convince his dad that he actually needs to stay 7 days to finish his antibiotics."
Praise God for this miracle. And for donors like you who gave so that this boy could have the gift of life.
6 Ways We Are Reaching the Poorest of the Poor
 Being a mission hospital means taking care of the poor. We are commanded to do this by Jesus, and it is something we desire to do. If we offer free care, we will be inundated with patients. How could we possibly treat them all? If we charge for the care, we may overlook many who are very poor. What can we do?
Being a mission hospital means taking care of the poor. We are commanded to do this by Jesus, and it is something we desire to do. If we offer free care, we will be inundated with patients. How could we possibly treat them all? If we charge for the care, we may overlook many who are very poor. What can we do?
- First, everyone is expected to pay something. Even if it is only a few cents. It is simply not sustainable for us to provide free care. Indeed, most Africans have a social safety net made up of family, friends, church members, etc. who can contribute to their medical expenses. However, we recognize that this will not be enough for some patients. For them, we have a Benevolent Fund that can cover their costs.
- We have a committee of nationals who evaluate patients and their eligibility for the Benevolent Fund. In a country like Ethiopia, where many in the population live on less than $1 per day, it can be difficult to sort out who are the poorest among the poor. Particularly for Westerners working here. Relative to our background, everyone seems poor, and we would likely put everyone on the Benevolent Fund. That is why it is so crucial to have nationals evaluate these situations on a case-by-case basis.
- We lower costs as much as possible by using expatriate specialist staff who are funded separately through their respective mission agencies. We still have to pay for all the operating costs of the hospital, the nursing staff, our national doctors, and supplies. But we offset these costs with donations and some volunteer staff. Much of our equipment is donated which lowers capital expenses for the hospital and this is passed on to patients.
- The rural poor in Africa have less than a 10% chance of seeing a doctor in their lifetime. The medical services simply do not exist for the vast numbers of people. (Ethiopia alone has close to 100 million inhabitants.) Ultimately, it comes down to training. We are training surgeons, physicians, medical students, and nurses. If we are truly going to expand our reach to the poorest of the poor, we must increase capacity in the face of such great need.
- We are going out into the community with Community Health Evangelism, Helicopter Outreaches to the T'ara people, and rural prenatal clinics. These initiatives are taking the Gospel and quality medical care to rural poor who would otherwise never see a a doctor.
- Your donations make a difference. As we have written on here before, 96% of the money you give on this site, goes directly to Ethiopia. A significant portion of that goes to the Benevolent Fund. Which in turn pays for care for the poorest of the poor.
Click here to give today, and know that you are giving to an organization that is doing all it can to reach "the least of these."
12 Things for Non-Doctors to do at SCH

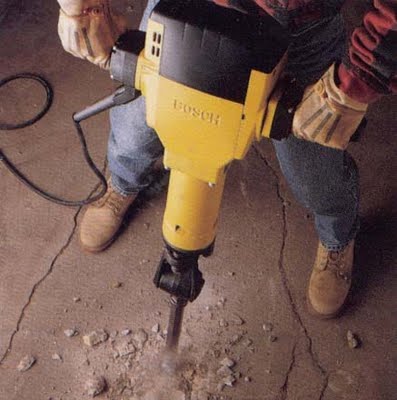
Okay, so we're not gonna ask you to jackhammer (unless you really want to). But one question we do get a lot is: "I'm not a doctor. Could I still be of any use at the hospital?" So here are 12 things that you could do at the hospital if you are not, say, medically inclined...
1. Plumbers & electricians: We need all sorts of skilled labor done around the hospital. We have septic systems, generators, and a myriad of other equipment that need tending to.
2. Leadership development: Are you a manager or have experience coaching leaders? Come and help us train our senior staff at the hospital.
3. Teachers: You can teach English at our hospital language school. We also have about 15 missionary kids (MK's) here in addition to our residents' kids, and they would love a Vacation Bible School or some type of sports camp. That means you too, coaches.
4. Organizers: Are you organized? We have loads of equipment and materials that need to be inventoried/cataloged. Come and get your type-A personality fix here!
5. Office computer skills: Are you good with Excel? Want to host a workshop for our financial people? What about Word or other clerical software? We have a large administrative staff that you could train.
6. Any IT/Networking People out there? We recently began a network at the hospital, and are running a server and handful of workstations. What's next? Come help us figure it out, and figure out ways to run our network better.
7. Prayer partners. Would you want to pray with some of our patients? Maybe hold a child's hand before they go into surgery?
8. Babysitters: Our missionaries need a break every once and a while. Perhaps you could watch their kids, so they can go out for dinner.
9. Artists: Want to come and paint some cool murals on our hospital walls? Or how about do some art with the patients or the MK's? Give us your ideas, and let's do it.
10. Chefs/restauranteurs/amateur cooks: We cook everything here from scratch, so it's a lot of work! How about you come and help teach us and our staff how to prepare simple meals from scratch from our locally available ingredients? Or just cook for us, and give us a break with your delicious home-cooked meals!
11. Pastors/church leaders - Come and work with our chaplains and train/work alongside them!
12. Anything you want to do! - This place is ground-up work, and there are all kinds of tasks to do. How has God gifted you? Just ask us, and let's figure out a way to use those gifts here!
What's Your Specialty?
At Soddo Christian Hospital, we offer all types of general and specialized care. Here's a sampling of specialized services that we offer at Soddo Christian Hospital:
- We have an outpatient department with an emergency room and non-urgent primary care. We see pediatric and adult patients. Our general medical staff includes a US-trained pediatrician, emergency physician, family nurse practitioner, and tropical disease expert. We have a European-trained geriatrician, as well as a national internal medicine specialist who sees clinic patients and inpatients.
- We have two, that's right TWO, US-trained general and trauma surgeons. They serve as the primary faculty advisors for the general surgery residency program at the hospital. (Yes, we are a teaching hospital affiliated with the Pan-African Academy of Christian Surgeons). This team performs other surgeries as well including a fair amount of urologic procedures.
- Orthopedic Surgery - we have a US-trained orthopedic surgeon and perform a full gamut of bone and joint surgeries with pediatric and adult patients, including arthroscopic surgery!
- Obstetrics & Gynecology - our US-trained obstetrician and team of midwives perform deliveries and C-sections as well as expert gynecology services.
- Subspecialties are available on an occasional basis. Through World Medical Mission, we have plastic surgeons, ENT (ear, nose & throat), urologists, and neurosurgeons come and work in Soddo on a frequent basis.
As you can see, we are well staffed to take care of all types of emergent and non-emergent conditions!