Yellow Fever near Soddo
We have bad news and good news…
The bad news: there has been an outbreak of Yellow Fever in our region of Ethiopia, affecting about 35 people and killing 10.
The good news: Three of Soddo Christian Hospital’s staff members were instrumental in identifying the disease and reporting the outbreak to the World Health Organization, leading to the shipment of 1.5 million doses of the vaccine to Ethiopia.
 The discovery of the outbreak began when a patient showed up at our hospital with all the classic symptoms of Yellow Fever. But since that virus has not been present here in recent history, clinicians were hesitant to identify it as such right away. However, the next day another patient presented with similar symptoms and died. Then other patients at the hospital began telling our staff stories about people dying in a certain town – three of them in the same family!
The discovery of the outbreak began when a patient showed up at our hospital with all the classic symptoms of Yellow Fever. But since that virus has not been present here in recent history, clinicians were hesitant to identify it as such right away. However, the next day another patient presented with similar symptoms and died. Then other patients at the hospital began telling our staff stories about people dying in a certain town – three of them in the same family!
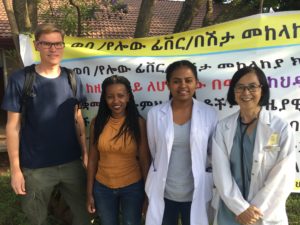
That’s when Dr. Ribka, Dr. Sok, and Nurse Woynishet reported their suspicions to the Zonal Health Officer, even though it was late on a Saturday night. Immediately, the CDC, WHO and UNICEF got involved with investigating, documenting and testing. Yellow Fever was indeed the confirmed diagnosis.
Photo L to R, Dr. Joakim, missionary infectious disease specialist from Sweden; Nurse Woynishet, works in ER and is responsible for reporting infectious diseases to health officials; Dr. Ribka, general practitioner; Dr. Sok, missionary internal medicine specialist.
 Thanks to the astuteness and persistence of our staff, 1.5 million Yellow Fever vaccines are now in Ethiopia. Our hospital is one of the immunization sites, having already immunized nearly 1,000 people since last Friday.
Thanks to the astuteness and persistence of our staff, 1.5 million Yellow Fever vaccines are now in Ethiopia. Our hospital is one of the immunization sites, having already immunized nearly 1,000 people since last Friday.
We are so very proud of our staff for acting quickly, containing the outbreak, and saving many lives!
Dr. Sok updating the SCH medical staff about the Yellow Fever outbreak and the containment strategy
The official news story at: https://in.reuters.com/article/us-ethiopia-yellowfever/yellow-fever-kills-10-in-ethiopia-who-ships-1-45-million-vaccines-idINKCN1NA2K3
Our wonderful staff: Giving back however they can
 One of our recent visiting residents wrote about his week at Soddo Christian Hospital this summary of his visit:
One of our recent visiting residents wrote about his week at Soddo Christian Hospital this summary of his visit:
“We do what we can”
It takes a huge team to care for patients here. This picture is of the multidisciplinary team that makes orthopedic rounds each day. They do a wonderful job in very challenging situations. Our staff every day confront medical needs that challenge both their medical skills and their emotional fortitude. The orthopedic surgery resident from UCLA just finishing his week-long surgical rotation at Soddo summarizes his experience below.
“It’s been a tough week here. There are so many people that come to Soddo Christian Hospital from all over the eastern part of Africa and Ethiopia, and there are only so many resources and only so much time in a day to help people. There is such an inundation of trauma from road traffic accidents, and [so many] infections [because of] people waiting to see physicians or travelling for days to come to this hospital, that the operating room is reserved for the [most] serious of emergencies. Emergencies that would be deemed emergencies in the United States are true emergencies here, too, but the timing of treating them is delayed, with a certain amount of triage that [must occur]. For example, hip fractures are generally treated within 24-48 hours to reduce morbidity and complications from immobility and pain. [But] we’ve had a patient in the hospital who has had a hip fracture for 2 months, who arrived last week. He’s in need of hip implants, which are coming, but are waiting at customs in Addis Ababa. They should arrive next week.
“It’s hard to see patients in clinic who have real problems that are solvable with the right resources: osteoarthritis treated with knee or hip replacements, ACL or PCL injuries treated with arthroscopic reconstructions, or even basic fractures like tibias, femurs, forearms or elbows. Many are treated in a delayed fashion because of the need to take care of infections or open fractures. [See the two children pictured.] Many emergency patients sleep in the yard of the hospital waiting for a bed. It’s heart-wrenching to see children who can’t walk because of neglected, infected hips that have destroyed the joint, or complications from things like TB and polio, which are so rare in the US.
“Over the past week, we’ve had some complex cases. As a team, we were able to perform 2 complex pelvic operations; a scapula/glenoid fracture was fixed, as well as multiple open femur and tibia fractures, along with a few pediatric fractures due to traffic accidents. Additionally, we had a couple of patients with multiple knee ligament injuries. Given my interest in sports medicine, and the presence of an arthroscopy tower in the OR (one of the few in the country), Dr. Anderson challenged me to take care of a couple of the knee ligament injuries and expose the Ethiopian residents to arthroscopy. I quickly realized that arthroscopic surgery here would be extremely challenging: the language barrier, the power goes out frequently, [and] the staff is used to dealing with trauma [injuries so] all [the] arthroscopic instruments are new [to them]. Additionally, these injuries were difficult as multiple ligaments were injured, and we would be reconstructing multiple ligaments at a time. [Seeing my hesitation], Dr. Anderson motivated me by explaining that we were likely the only people in Ethiopia who had the equipment and the ability to treat these injuries.
 “[W]e ran 4 operating rooms at the same time. One Ethiopian resident took consults in the Emergency Room, one Ethiopian resident operated on infections and long bone fractures, Dr. Anderson and another Ethiopian resident fixed a complex pelvic fracture, and the fourth Ethiopian resident helped me with [the] arthroscopic PCL reconstruction and used the fluoroscope machine to fix a complex tibia fracture. We all made it through. And when we were done, the knee felt stable, the pelvis was fixed, and 8 other infected bones and fractures were clean and fixed. It was a tough, long day, but in retrospect, we accomplished a lot as a team.
“[W]e ran 4 operating rooms at the same time. One Ethiopian resident took consults in the Emergency Room, one Ethiopian resident operated on infections and long bone fractures, Dr. Anderson and another Ethiopian resident fixed a complex pelvic fracture, and the fourth Ethiopian resident helped me with [the] arthroscopic PCL reconstruction and used the fluoroscope machine to fix a complex tibia fracture. We all made it through. And when we were done, the knee felt stable, the pelvis was fixed, and 8 other infected bones and fractures were clean and fixed. It was a tough, long day, but in retrospect, we accomplished a lot as a team.
“As I reflect on my last day operating here, I think there’s a bright outlook for this country. I’m encouraged that I helped expose the Ethiopian residents to arthroscopic surgery. I feel grateful to see that [my supervising doctors] have trained me to perform these cases independently. Lastly, I was very impressed with the Ethiopian residents. They are smart and extremely well read. Dr. Anderson’s knowledge and ability is impressive. Soddo Christian Hospital’s resources, though limited compared to the USA, provide an orthopedic mecca for the Ethiopian residents here. I’m hopeful that the partnership with UCLA/OIC can continue to bring US residents with different interests to Ethiopia where we can learn from Dr. Anderson and the residents—and give back however we can.”
Surgical Treatment of Chronic Elbow Dislocation Allowing for Early Range of Motion: Operative Technique and Clinical Results
Surgical Treatment of Chronic Elbow Dislocation Allowing for Early Range of Motion: Operative Technique and Clinical Results
This is the largest case series of surgically treated patients with chronic elbow dislocation. Using our surgical technique, 97% of patients had good or excellent outcome with a low complication rate. Open reduction of chronic elbow dislocation can be accomplished while permitting early motion with minimal recurrent dislocation risk.
We have developed a straightforward surgical technique that allows for early elbow range of motion (ROM) with a little risk of recurrent instability. We present the operative technique and results of this surgical technique from 2 tertiary centers in Ethiopia. Our hypothesis is that our surgical technique and postoperative rehabilitation protocol allows for good patient outcome regardless of injury duration.
Duane R. Anderson, MD,* Justin M. Haller, MD,† Lucas A. Anderson, MD,† Samuel Hailu, MD,‡ Abebe Chala, PT,* and Shawn W. O’Driscoll, MD, PhD§
Teamwork at SCH
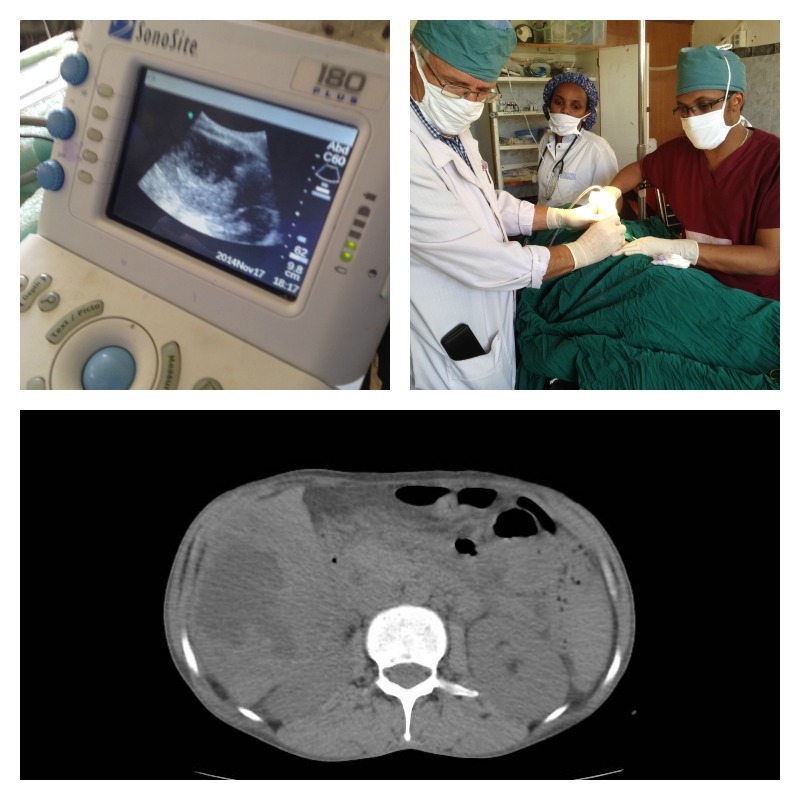
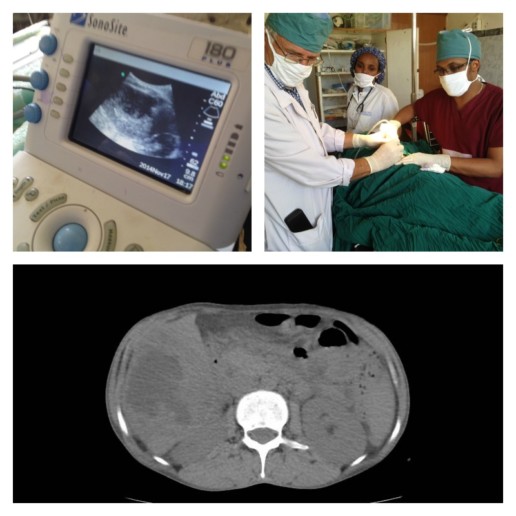
As our capabilities at Soddo Christian Hospital expand, we are working together as a team to make diagnoses, and provide cutting edge treatment for patients. The other day, we had a woman present to the Emergency Room with upper abdominal pain and fever. The ER docs did a great job with the bedside ultrasound finding what appeared to be either a fluid collection or a mass in her liver (top left picture). Then, a CT scan by the Radiology Department confirmed that it was indeed an abscess in the liver (lower pane). Finally, our expert radiologist teamed up with our surgeons (that's our chief resident Dr. Segni in the top right picture) to do an ultrasound-guided percutaneous drain. This is a minimally invasive way to get the infection out instead of a big operation.
We are so proud of all of our services working together to get the best outcomes for patients! Praise God for new technologies and teamwork!
[ois skin="Blog Post Share"]
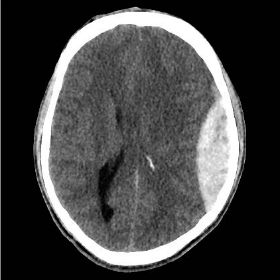
Neurosurgery at SCH?!?
What do you think happens when you combine the following:
- A country with the highest number of pedestrians struck by vehicles relative to cars on the road
- A brand new CT scanner among a population of 5 million people who previously had none
If you answered, “a lot of new diagnoses of head trauma”, you’d be right. Our CT scanner is practically smoking with all the head CTs for trauma that are being done. Most of the time, we find non-operative bleeds. But the last two weeks has been extraordinary. In September alone, we have taken seven patients to the OR with epidural and subdural hematomas that required emergency surgery.
 Above are just four of the actual scans done here in the past two weeks. And there are more! We’ve had great outcomes so far, and our surgery residents and staff are doing more emergent neurosurgery than they ever could have imagined.
Above are just four of the actual scans done here in the past two weeks. And there are more! We’ve had great outcomes so far, and our surgery residents and staff are doing more emergent neurosurgery than they ever could have imagined.
We praise God that He provided through our donors. Through your generosity, we got a CT scanner. And it is being used for His glory as lives are being saved. May the name of Christ go forth in southern Ethiopia as we use this gift. That is our prayer.
Empowering the Next Generation
Imagine a missionary doctor sitting under a tree in Africa, seeing patients as they line up from far and near. She sees 100 patients a day or more. In a year, perhaps 3000. In ten years, 30,000. Not a bad contribution to the problem of suffering in her country. But imagine how burned-out, how completely exhausted she is after this work. And when she finally gives up, the work is finished. Many thousands of patients were treated, and many lives saved even. But the work is not enduring. It is not sustainable.
Now, imagine that same doctor pouring her life into doctors-in-training in that country. Year after year, spending intentional time teaching 10-15 resident physicians. In ten years’ time, perhaps 20 or 30 are trained. Each of those go on to treat thousands of patients in their careers. Some of them are retained as teaching physicians, and they in turn pour into others. This is multiplication. This is empowerment. The impact of that one person is perhaps 50-fold when compared to the lone worker at the beginning of our story.
This is what we do at Soddo Christian Hospital through PAACS.
The Pan-African Academy of Christian Surgeons was founded in 1996 with one residency program in the jungles of Gabon. Since then, it has grown to twelve programs in ten countries. We are one of those programs. Why is it so important to train African surgeons?
Right now, 56 million people in sub-Sahara Africa are in need of surgery. In most of the continent, there is one surgeon for every 250,000 population. In Ethiopia, there are only a 300 surgeons for a country with almost 90 million inhabitants. (If WHO guidelines were met, we would have 4,150!) PAACS has the goal to train 100 surgeons by 2020. Thirty-six have been trained thus far, and God-willing, the goal will be met by 2019.
Because the program is fully accredited, our graduates are eligible to be members of the College of Surgeons of East, Central, and Southern Africa. And in turn, are fully licensed by the country of Ethiopia as surgeons. And the faculty actively disciple the residents during their training - teaching them not just excellent surgical practice, but equipping them with the spiritual tools to use medicine to bring people to Christ.
We praise God for this kind of empowerment and training. Of Africans. For Africa.
Battling the Brain Drain
What is the “brain drain” anyway? In developing countries all over the world, the “brain drain” refers to the tendency of qualified and skilled workers to leave the country in search of greener pastures. To America, to Europe. The salary of a physician in the USA may be 100 times that of his counterpart in the developing world. Is it any wonder that so many leave?
And yet, the consequences are felt by the countries they leave behind. The people in those countries long for skilled engineers to design their infrastructure. For skilled physicians and surgeons to treat their medical problems. For talented musicians and artist to elevate their culture.
In health care, the effects are especially acute. People’s lives are at stake. The minister of health for Ethiopia has even famously said that there are more Ethiopian physicians in Chicago than in Ethiopia itself! So the country is taking on the challenge head on. Thirteen new medical schools were opened in the past two years. But this just means more junior level doctors who will also be looking for the exits.
Unless…
We can train them in a specialty. You see, the vast majority of Ethiopian medical school graduates (general practitioners, or GPs, they are called) are looking to advance their education by further training. Just like in the US and other places, they want to do a postgraduate residency. Whether it’s Obstetrics/Gynecology, Internal Medicine, Radiology, Pediatrics, or whatever. They are not content to be only graduated GPs. They want that further training.
And so, Soddo Christian Hospital is actively battling the brain drain as well. We have a five year General Surgery residency that is fully accredited by Ethiopia’s Higher Education Authority and COSCESA – the College of Surgeons of Central, East, and South Africa. We are actively discipling them with the Word of God. As they study Jesus’ heart for the “least of these”, they are motivated to use their skills to alleviate the crisis in their own nation. Not leave for another country. Yes, that's right. Our graduates stay in Ethiopia! And so, we see Dr. Frehun in Addis, and Dr. Haile in Asela and Dr. Tedi here in Soddo training more surgeons. By God’s grace, all of our graduates have stayed home!
We’ll tell you more about PAACS and how this organization is helping not just Ethiopia, but all of Africa, in the next post…
SCH Graduate Makes History
Recently, the very first graduate from the PAACS program in Ethiopia did something unique in his own country. He led a team that separated conjoined (“Siamese”) twins. To our knowledge, nothing like that had ever been attempted in Ethiopia. Dr. Frehun Ayele, who trained as a pediatric surgeon at the BethanyKids at Kijabe Hospital PAACS program after graduating from the general surgery program in Ethiopia, led a team of surgeons from Myungsung Christian Medical Center to perform the incredibly delicate and complicated operation. The baby sisters were born at a health center in the countryside and were abandoned by their mother. They were given to a Catholic mission group here who then brought them to MCM. One of the twins had a severe, fatal heart defect and it soon became clear that she could not survive. This made transfer abroad impossible because of time considerations, so Frehun made the difficult decision to take them to the operating room to separate them. It was clear that one of the twins would die, sacrificing her life for her sister's. Dr. Frehun concluded that if he did not intervene urgently, both babies would die. The surviving twin, Mariam, is doing well. Please pray for her as she recovers. We praise God for Frehun's faithfulness in serving Him as he serves the sick children of Ethiopia.


Welcome Home!


There's no place like home! And now, after many years of prayer and preparation, the new Soddo PAACS apartment building is complete, and our residents have moved in to their new homes.
The finished building has 7 apartments (1 three-bedroom, 3 two-bedrooms and 3 one-bedroom apartments). These new apartments will allow the surgical residents to have a reliable source of power and water. And, since they are on the hospital's campus, it will significantly improve their home security, including that of their families. From an educational standpoint, this will also allow us to improve the residents' experience with night call. This will allow senior residents to take back-up call in the night and gain experience in teaching junior residents under faculty supervision in the night hours.
We want to extend our deep appreciation to everyone who gave so graciously to make this happen. We have been encouraged by everyone's support and gifts, even in the end as we raised money to furnish each apartment. A big thank you goes to Africa Mission Healthcare Foundation for their donation that funded over a third of the project costs!
The residents are enjoying living in the same building and often eat together, sing praise music together and enjoy holidays together since they are away from their extended families. Dr. Surafel said, "Living on-campus together gives us lots of time for fellowship and we eat many meals together. It is also easier to see patients more quickly."

playground!

White Coat Ceremony
What is a white coat ceremony, you ask? Well, according to Wikipedia, it is the ritual that marks the transition of a student of medicine from the pre-clinical years to the clinical years. The white coat has been worn for over 100 years by medical professionals, and is clearly associated with the trade. Everyone likes ceremonies, and for doctors, this is an important ritual that bestows the rights as wells as responsibilities on new doctors.
Though typically done with medical students, we have developed our own version of the white coat ceremony for our PAACS residents. Performed as they begin their five year training, we assemble in the chapel here at Soddo Christian Hospital and deliver a charge to the new young surgeons. This past week, we welcomed Dr. Gezahegn and Dr. Ebeneezer into the ninth class of surgical residents here. Here is how it happened:


The time was opened with a song and prayer led by Pastor Daniel, SCH’s head chaplain. Then Dr. Gray read John 13 reminding all of the servant leadership by Jesus and do likewise. “For I have given you an example – you should do just as I have done for you.” John 13:15. Dr. Mark Karnes shared his prayer for the residents from Colossians chapter 1. He charged them with 3 important things to remember throughout their training. First, God is in control; rest and trust in this. Second, treat all patients with care and compassion as if they were family. Third, know your limits and don’t be afraid to ask for help.
Next, Dr. Seigni Bekele, SCH’s chief resident encouraged the interns with some scripture and words of wisdom. He read from Hebrews 12:1-2, mentioning the men of faith that are listed in the chapter before this. He emphasized that there are many people of faith who pray continually for PAACS and for the residents here. He challenged the interns to remember they are a part of something great and many people have gone before them in sacrifice and prayer to get the program to where it is today. And for that we are thankful and give glory to God. “Keeping our eyes fixed on Jesus, the pioneer and perfecter of our faith.” Hebrews 12:2

Dr. Gray spoke last pointing out that in order to be the greatest we need to be the least. And that the desire in us to be the greatest is not wrong, but it is what we are aiming for that makes the difference. If we stay focused on eternity and we strive to do well for the eternal, then the world may consider us crazy, but we will know we are aiming for something great.
Finally, following Jesus' example from John 13, Dr. Karnes and Dr. Gray washed the feet of Dr. Gezahegn and Dr. Ebenezer. Not something you'd find in most white coat ceremonies, but servant leadership being the focal point of our training, a practice that we feel is essential to this rite of passage. As staff physicians, we want to model servant leadership to even our newest trainees, as we begin to mentor them. A blessing was prayed over them as we concluded the ceremony.